New Study Shows Doctors Prescribing Lower Dosage Opioids

At this point, it is no mystery that the opioid addiction epidemic that has claimed hundreds of thousands of lives began largely by doctors overprescribing highly addictive pain medication. With that in mind, it makes sense that many doctors are now becoming more conservative in prescribing.
But are doctors going far enough? And are they offering alternative pain relief options to their patients? While a reduction in the prescribing of opioid pain relievers for post-operation pain is a step in the right direction, it should be followed by physicians prescribing nonopioid pain relief treatments as alternatives. Doctors should prescribe opioid pain relievers only as a last resort after other, safer pain relief methods have been attempted.
New, Positive Developments in Opioid Prescribing
One study presented at the ANESTHESIOLOGY® 2022 annual meeting showed that, while there has been no decrease in the overall number of opioid prescriptions patients are being given by doctors following surgery, the dosages of opioids in those prescriptions have gone down. That indicates doctors are more mindful of the potency of the drugs they prescribe to their patients. It indicates that doctors are opting for less potent prescriptions to avoid the risk that their patients may become addicted to the drugs that are supposed to help them recover.
The research showed that, just as the prescribing of high-dosage opioids declined, figures for patients seeking nonopioid pain relief went up (over-the-counter medications such as acetaminophen). For example, in 2013, at the height of opioid prescribing, only 9% of post-surgery patients bought acetaminophen. But by 2017, 28% of patients sought the over-the-counter pain reliever. The researchers theorized that patients were increasingly turning to OTC drugs as a relief supplement because they were being prescribed lower-dosage opioid pain relievers by their doctors.
That may be a positive development, but the truth remains that most patients were still receiving opioids, even if in lower doses. (In 2013, 76% of the patients in the study group were prescribed opioids, which only dropped to 75% by 2019). While potency does make a big difference in addiction risk, any opioid prescription puts the patient at some risk of developing an addiction.
Still, doctors have been prescribing opioids in less potent doses, and the researchers were pleased to present their findings regarding that shift. According to their data, the decrease in potency went from an average of 317 MME (morphine milligram equivalent) in 2013 to an average of 260 MME in 2019.
The researchers also indicated that more needed to be done to curb opioid prescribing while simultaneously offering patients other options. Quoting Dr. Naheed Jivraj, lead author of the study and a critical care medicine fellow at the University of Toronto, Ontario, “While it’s good news that the doses in opioid prescriptions are being reduced, the fact that the actual number of opioid prescriptions filled has remained the same shows there is still an opportunity for improvement.” While opioid painkillers can be an important part of pain management, such drugs are highly addictive no matter what dosage is prescribed, and prescribers must consider that.
What the CDC Prescribing Guidelines Recommend

The Centers for Disease Control and Prevention have released several guidelines regarding opioids. While their most recent edition focuses on many medical fields and a wide range of medical specialties, their original release, a 2016 edition, focused solely on primary care physicians, which is most relevant here. According to those guidelines, the CDC encourages doctors to only prescribe opioid pain relievers after other nonopioid pain treatment methods have been attempted.
Further, the CDC recommended that if opioids are to be used, clinicians should only prescribe immediate-release opioids instead of extended-release opioids and that “Clinicians should use caution when prescribing opioids at any dosage, should carefully reassess evidence of individual benefits and risks when considering increasing dosage to ≥50 morphine milligram equivalents (MME)/day, and should avoid increasing dosage to ≥90 MME/day or carefully justify a decision to titrate dosage to ≥90 MME/day.” The recommendations indicate that clinicians should avoid prescribing opioids for more than three to seven days.
Given the rising awareness of the addiction risk of opioid pain relievers and the increasing pressure on physicians to either prescribe lower doses of opioids or to avoid prescribing opioids completely, physicians will need to offer their patients alternatives.
Thankfully, alternatives do exist. Doctors can work with their patients and attempt nonopioid pain relief treatments like:
- Pain pumps
- Acupuncture
- Radio waves
- Physical therapy
- Massage therapy
- Electrical signals
- Spinal cord stimulation
- Injections or nerve blocks
- Changes in diet, sleep or exercise patterns
Every patient’s case will be different and unique to them. That’s why patients recovering from acute, short-term, post-surgery pain, or chronic pain should talk to their doctor about how to treat pain without opioids.
Why is There a Need for Prescribing Alternative Pain Relief Options?
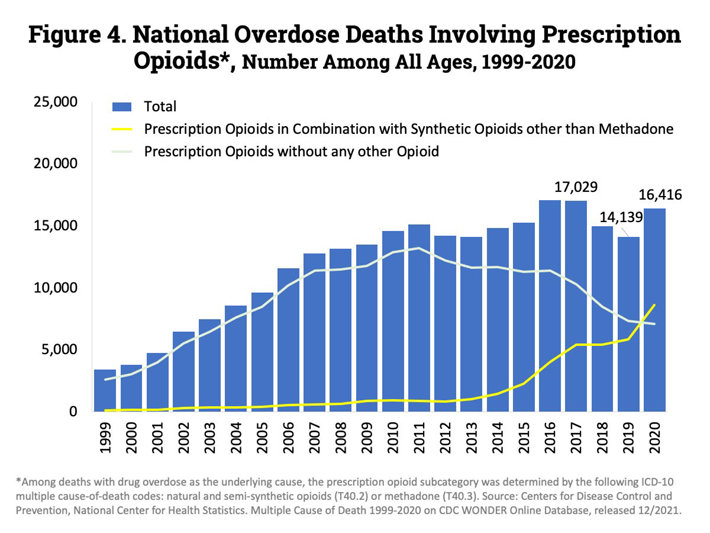
According to the National Institute on Drug Abuse, overdose deaths from prescription drugs have been rising almost non-stop, year after year, since the 1990s. In 1999, around 3,000 Americans lost their lives to prescription opioid overdoses. But in 2017, when fatality figures peaked, more than 17,000 Americans died. About 16,400 lost their lives in 2020, with 2021’s figures expected to be worse.
Sources:
- CDC. “Understanding the Opioid Overdose Epidemic.” Centers for Disease Control and Prevention, 2022. cdc.gov
- ASA. “Opioid prescribing after surgery remains the same for seniors, but doses are lower, study shows.” American Society of Anesthesiologists, 2022. asahq.org
- CDC. “CDC Guideline for Prescribing Opioids for Chronic Pain.” Centers for Disease Control and Prevention, 2016. cdc.gov
- ASA. “Nonopioid Treatment.” American Society of Anesthesiologists, 2022. asahq.org
- NIDA. “Overdose Death Rates.” National Institute on Drug Abuse, 2022. nida.nih.gov


 ®
®